Stainless Steel 304: Comprehensive Analysis of Performance, Applications, and Selection Guide
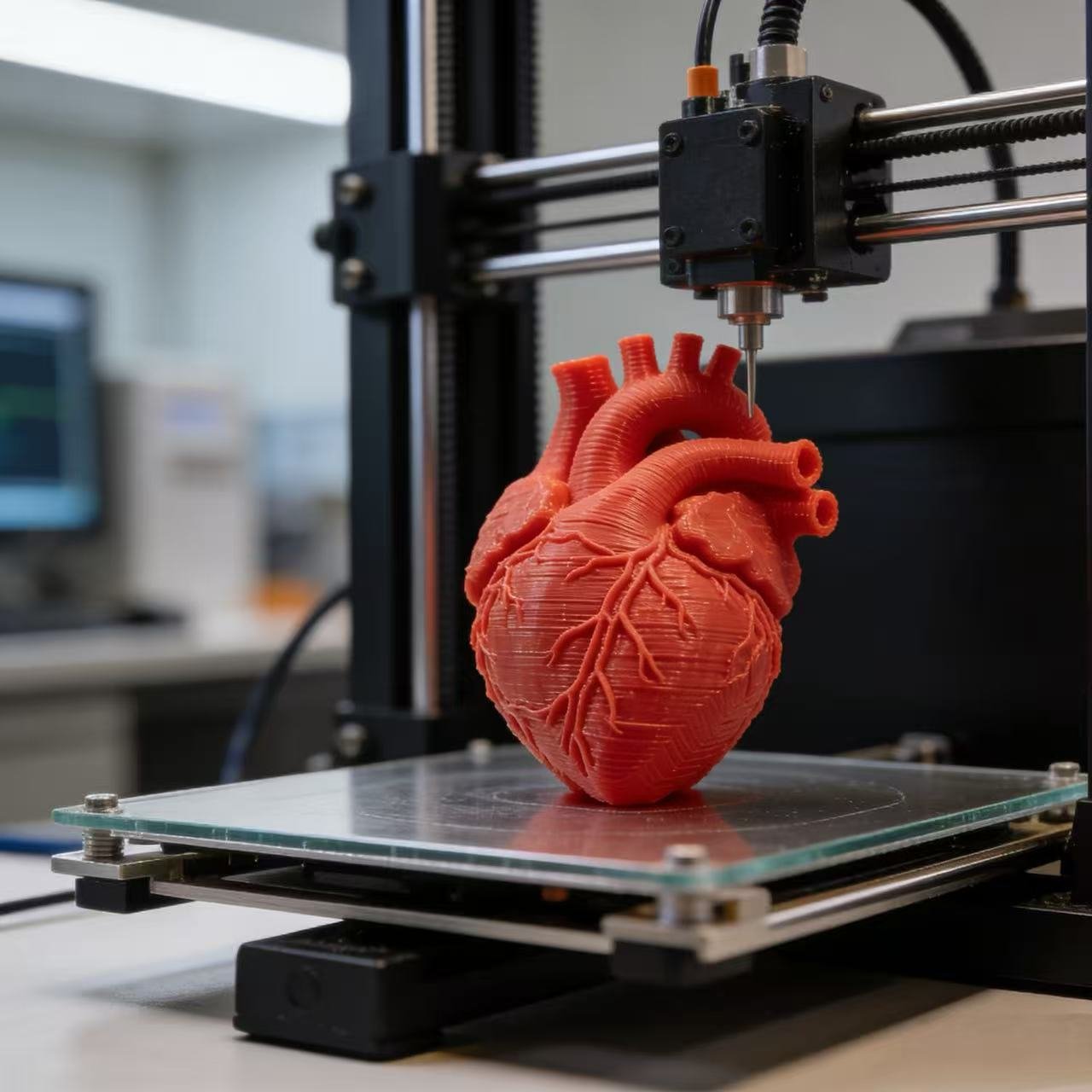
Step into a modern kitchen, open a refrigerator, walk into an office building elevator, or observe medical equipment—in these seemingly different scenarios, one material silently underpins our lives: Stainless Steel 304. As the most common and widely used grade of austenitic stainless steel, SS304 has become an “invisible champion” in industrial manufacturing and daily life, thanks to its excellent corrosion resistance, good formability, and outstanding hygienic properties.
Since stainless steel was invented in the early 20th century, 304 stainless steel has evolved into the world’s most popular stainless steel variety, accounting for approximately 50% of the stainless steel market share. From aerospace to food processing, from architectural decoration to medical devices, this alloy occupies an irreplaceable position in modern materials science due to its unique combination of properties. This article will provide a comprehensive analysis of the chemical composition, mechanical properties, application fields, processing techniques, and selection guidelines for 304 stainless steel, offering a thorough reference for engineers, designers, purchasers, and general consumers.